Featured
 Otte described her first quarter experience with taking courses online as an “adjustment.” She got used to the learning platform and learned how to pace herself. While managing a busy full-time position, she tackled the doctoral program. She is truly grateful for the times she interacted with and been guided by the faculty throughout the program. The faculty made sure she received the most value out of the assignments.
Otte described her first quarter experience with taking courses online as an “adjustment.” She got used to the learning platform and learned how to pace herself. While managing a busy full-time position, she tackled the doctoral program. She is truly grateful for the times she interacted with and been guided by the faculty throughout the program. The faculty made sure she received the most value out of the assignments.
“There were always opportunities to collaborate with the faculty to tailor the assignments to be meaningful to my full-time job. The overlap really helped make the program more manageable,” she said.
If you are interested in the DMSc program, Otte suggests making sure that the educational experience and content are useful to your current or future career. The program is short, but a lot of work is required to make it through! Once you are in the program, find your rhythm early. Determine the times you can think clearly and work on your assignments every week. This will make your journey less stressful and you will be less likely to forget an assignment.
Otte is not motivated by titles, but by making a difference. She wants to help make the PA profession more diverse and encourage more PAs to work in underserved communities for the long term.
“The DMSc program has helped me expand my network of PA educators and allowed me to put the knowledge I gained directly into practice,” she said.
While in the program she has enjoyed how applicable the coursework has been to her daily job. Otte commented, “the program has caused me to think more critically in areas that I ordinarily wouldn’t have made time for.” She feels the program has created an added depth to her thought processes.
Otte is currently the founding program director of the Keck Graduate Institute Master of Science in Physician Assistant Studies (MSPA) program, which is located in Claremont, California. She oversees the development and long-term maintenance of the program, as well as ensures that the program remains compliant with accreditation standards.
As for balancing work, life, and self-care, Otte found it “rather difficult at times, but it did get better as I went through the program.”
“Working with faculty to tailor assignments was definitely helpful because my efforts were going towards both work and the program at the same time. Planning ahead and scheduling breaks for myself was really important,” she said.
Learn more about the PA education concentration Otte completed.
Archives
 Christine Bruce is an associate professor at The Pennsylvania State University’s physician assistant program and the program’s inaugural program director. Cynthia Chuang from Penn State’s Department of Internal Medicine has shared that Bruce is the “New England Journal of Medicine” deputy director of PA learners. Bruce is also the author of “Clinical Medicine for Physician Assistants,” 1st Edition. She has recently returned to full-time practice in primary care at St. Luke’s University Health Network at a rural, underserved medical site in her community. The doctors listed below were contributors to this recently published textbook.
Christine Bruce is an associate professor at The Pennsylvania State University’s physician assistant program and the program’s inaugural program director. Cynthia Chuang from Penn State’s Department of Internal Medicine has shared that Bruce is the “New England Journal of Medicine” deputy director of PA learners. Bruce is also the author of “Clinical Medicine for Physician Assistants,” 1st Edition. She has recently returned to full-time practice in primary care at St. Luke’s University Health Network at a rural, underserved medical site in her community. The doctors listed below were contributors to this recently published textbook.
- John P. Bastin ’19 DMSc, MHS, PA-C is currently an assistant professor/PA principal faculty at Florida State University’s College of Medicine. Bastin has been a PA for 27 years, and graduated from the U.S. Navy PA program in San Diego, California. He has experience in emergency and disaster medicine, so his background in those areas adds to his advancement of clinical experience in the PA profession.
- Benjamin J. Smith ’19 DMSc, PA-C, DFAAPA is currently the interim program director, associate dean, and associate professor of physician assistant practice at Florida State University’s College of Medicine. Smith is a distinguished member of the physician assistant profession with an extensive list of accomplishments to round out his career in clinical medicine.
- Brigitta Cintron ’19 DMSc, CTTS, PA-C has publications related to tobacco treatment. She has also taught courses in the certification of tobacco treatment. As a founding faculty member at Florida State University’s College of Medicine and a current full-time psychiatric PA, Cintron has made a significant contribution to the medical community. She is also currently teaching a few courses in Butler University’s Doctor of Medical Science program.
 Q: Congratulations on your new role as co-chair of the Diversity, Equity, and Inclusion Committee for the North Carolina Academy of Physician Assistants! What are you excited about in this new role?
Q: Congratulations on your new role as co-chair of the Diversity, Equity, and Inclusion Committee for the North Carolina Academy of Physician Assistants! What are you excited about in this new role?
A: This new role is very exciting for a few reasons. First of all, this is my first experience in a PA leadership position. I am very excited about the opportunity to give back to the PA profession!
Also, the focus on diversity, equity, and inclusion is near and dear to me especially being an African-American female. Often in academic or professional settings, I was the only person of color in a room. At times I was uncomfortable, yet I was mindful of my actions or appearance to make sure I did not make anyone else uncomfortable. This is why diversity and inclusion are so important. Especially inclusion. Everyone should feel welcomed, respected, seen, and heard. They should feel comfortable being who God created them to be. I realize how much representation does matter, across all areas — including, of course, the PA profession.
Q: What are the goals of the committee?
A: We have several!
1) We will focus on helping improve diversity within the profession. We planto engage with historically Black colleges and universities on recruitment, resulting in more diverse populations going into the PA profession.
2) We plan to develop continuing medical education (CME) on healthcare disparities. Oftentimes, these disparities are related to socioeconomic and environmental disadvantages. So our goal is to be able to identify where those disparities are and offer CMEs on those topics – related to COVID-19, HIV, and other issues. The goal is to mitigate these disparities.
3) We will offer implicit bias training to the NCAPA board members, and offer ways to look at our own respective biases. Of course, we will start within our committee of 10-12 members, and then we would like to take it outward to the other board members. We are very excited about the work we plan to do and the potential for change in these areas!
Q: What opportunities do you see for the PA profession to increase access to care for patient populations, and to reduce healthcare disparities?
 A: We as PAs are vital to the healthcare team and collaboration is vital. Also, we must mirror the populations we serve. It is so important to recruit providers from diverse cultural backgrounds and racial ethnicities because we are treating a variety of patients. Diversity helps to improve the delivery of care and helps to foster better relationships with our patients. It is also necessary to show PAs from different backgrounds in all types of roles, at all levels — regional, state, and national organizations.
A: We as PAs are vital to the healthcare team and collaboration is vital. Also, we must mirror the populations we serve. It is so important to recruit providers from diverse cultural backgrounds and racial ethnicities because we are treating a variety of patients. Diversity helps to improve the delivery of care and helps to foster better relationships with our patients. It is also necessary to show PAs from different backgrounds in all types of roles, at all levels — regional, state, and national organizations.
Q: Why did you want to become a PA?
A: Ever since I was a little girl, I was aware of my passion for helping and caring for others. I was very close to my grandmother, who suffered from chronic illness, and I helped care for her. I always made it a point to learn all her medications and what she needed. From that point, I knew I would become a healthcare provider.
I became a certified nursing assistant in high school and went on to undergraduate at University of North Carolina at Chapel Hill, where I learned about the PA profession in a Health Professions course. The flexibility of the profession and the available work-life balance within the profession drew me in. So I was accepted to Duke University’s PA program, where I graduated in 2009. I have worked in primary care, urgent care, and currently endocrinology, which I love!
Q: What are your career plans and goals?
A: I am excited to announce that I have been offered a position with Gardner Webb’s PA program as principal faculty. I will also be allowed to work one day a week, and I hope that I can continue working in endocrinology because diabetes care is an area where there are disparities in care. I enjoy working with my patients in Gaston County and surrounding areas and helping to improve their long-term outlooks.
Gardner Webb University is in Cleveland County (near Shelby, North Carolina) which is where I was born and raised. To my knowledge, I will be the first PA faculty member of color. This adds another level of pride and pressure. I want to do my part to have a meaningful impact on the program and pave the way for others like me. I’m thankful for the opportunity.
Q: Why did you choose to pursue the DMSc?
A: I am a firm believer in lifelong education. I always knew that I would return to education. A passion of mine is teaching and mentoring others — in this case, the next generation of PAs. I want to always inspire others. My motto has always been, “If I can do this, you can too! Believe in yourself, dream BIG, and remember all things are possible through Christ.”
I also felt like obtaining my doctorate would not only make me more knowledgeable in the topics that we studied, but it would also provide a whole new level of confidence. The PA profession is growing, and of course, I want to stay competitive. Many academic positions prefer that candidates have earned a doctorate, and this degree has helped me in that sphere.
Q: Any other projects you are excited about?
A: I have a passion for inspiring our youth. So I am planning to venture out on another journey – writing a children’s book. I have two young children of my own — the joy of my life! This book will be a fun read for children and parents!
 Becoming a teacher was a goal for Carl Garrubba since grade school, and his career in PA education has proven a natural fit. Garrubba enrolled in the DMSc due to the relevance of the curriculum for both his present job and also for the future.
Becoming a teacher was a goal for Carl Garrubba since grade school, and his career in PA education has proven a natural fit. Garrubba enrolled in the DMSc due to the relevance of the curriculum for both his present job and also for the future.
He is currently the program director for the PA program at the Dominican University of California in San Francisco.
“The DMSc is exactly what I was looking for. It gives me so much that I can use in my current program, but it has also given me so much that I can use for the future. That is exactly what I was hoping for, and never thought I would find it. I tell everyone that I talk with that this is the program that you need to do,” he said.
He has been drawn to both medicine and teaching his whole life, although he began his professional career as a CPA.
“I worked in public accounting, but I also worked in a university health center in the budgeting office. I made a lot of connections with the school of medicine there, and really enjoyed the conversations. At some point, I realized that being a CPA was not my true calling,” he said.
He had an enthusiastic PA friend who encouraged him to pursue the profession.
“I knew that I could hit the ground running after a few years of hard work, so that’s what I did,” Garrubba said.
He began his career in medicine at the height of the HIV crisis. He practiced in an HIV clinical research facility, when the HIV cocktail was new. He eventually worked in HIV primary care and managed a clinic for eight years.
“I did an eight-week rotation in HIV medicine, and knew I had to get involved,” he said.
Because he never gave up his dream of becoming a teacher and had an interest in PA education, he connected with a former professor from PA school when a job became available at Chatham University. He applied and was promoted to program director there.
“I love teaching. I love watching students learn. I love the ‘a-ha moments’ when they get it. I love to see them applying what they have learned, and the best part is seeing them in practice. I have run into students in medical settings, and that has been so rewarding. I love being a part of that process,” Garrubba reflected.
 After becoming a PA in her mid-thirties, working clinically and spending a few years in PA education, Hayhurst found Lynchburg’s DMSc through a colleague who was part of the program’s premier cohort.
After becoming a PA in her mid-thirties, working clinically and spending a few years in PA education, Hayhurst found Lynchburg’s DMSc through a colleague who was part of the program’s premier cohort.
“I discovered my niche within healthcare administration directly through my DMSc coursework. I found my bridge between PA education into helping current PAs see their worth within the practice, and helping advocate for them,” she said.
Hayhurst practices clinically and also serves as a director and resource for Advanced Practice Providers on issues of standard of care, duty to patients, and meeting risk management protocols within a large dermatology group in southern California.
“As PAs, even though there are so many of us, we are still a small community, and we need each other to help reach our full potential as a profession,” Hayhurst said.
She knew early on that she wanted to become a PA.
“When I was in high school, I worked for a local dermatologist, and there was a PA in the practice; the PA treated patients also. The PA profession wasn’t as well-known at that time,” she reflected.
After college, Hayhurst had a career in medical sales and marketing, but always had the goal of becoming a clinician. “It was always in the back of my mind — this was always my goal.”
“When you’re in PA education, you realize the value and importance of training up the next generation of PAs — you see your role in mentoring, bringing the profession up, and moving it forward,” she said.
Hayhurst said that having the support of her family has been key throughout her academic pursuits.
“My children were very young when I started PA school, and they were 10 and 13 years old when I began the DMSc. They were able to see me working hard toward my goal of receiving my doctorate. They would study alongside me, and I was able to show them the value of education. Seeing how proud they were of me was so meaningful,” she said.
“Another goal of mine, even after finishing PA school, was to earn my doctorate. I thought the DMSc was excellent. I thought — this would have been great to have this advanced knowledge in PA school. It helped build on the knowledge that I already had and took it to the next level.”
She noted that a favorite course was on healthcare law.
“I learned so much! The curriculum is very thoughtfully laid out and makes the workload doable, and maximizes what you can learn throughout the course without becoming overwhelmed,” she stated. “I enjoyed the balance of self-directed learning and the availability of having faculty mentors, Dr. Nancy Reid and Dr. Trey Boyd. They were always available for conversations and flexibility when needed, which goes right along with the PA profession. It’s what we do.”
 Lawrence (Larry) Herman ’20 DMSc, PA-Chas worked in the medical field for 30 years. He started out working in a busy trauma center in New York City. Then he went to the New York Institute of Technology (NYIT) to learn more about being a PA. He has also worked in PA programs across the southern United States.
Lawrence (Larry) Herman ’20 DMSc, PA-Chas worked in the medical field for 30 years. He started out working in a busy trauma center in New York City. Then he went to the New York Institute of Technology (NYIT) to learn more about being a PA. He has also worked in PA programs across the southern United States.
No matter where he has worked, he has been a leader. He served as the head of emergency medicine APPs at St. Vincent/Catholic Medical Center and then as director of clinical education and program director at NYIT. Herman was recruited to be program director and dean in North Carolina, and a program in Texas.
Herman has been a pharmacology teacher for 16 years. He was also a PA in emergency medicine and family practice. Herman has been very successful, holding national leadership positions including being the past president of the American Academy of PA and being a distinguished fellow with AAPA.
Herman has been working as a consultant in South Carolina for several years, helping PA programs with issues of accreditation and compliance. More recently, he has been working with medical education companies (MECs). He helps them figure out what their students need to learn and writes curricula for them. He also applies for grants based on specific diseases, like vaccines or cancer prevention. In this arena, one of his roles has been to moderate and serve as a content expert for continuing medical education (CME).
Herman moderates several continuing medical education (CME) programs for organizations likePrimed (Boston and Philadelphia) and the AAPA. In the past, this job required a lot of traveling. But now with more people using online platforms, Herman has been working to revise and rewrite important grants so they will work well on online platforms.
He said that he is used to giving presentations to audiences of 500 to 1,000 PAs. But, he was working on developing new ways to keep the audience’s attention by using the technology that is available now.
Herman is no stranger to developing technology. He has been involved in podcasts for Primed. The podcasts are designed for physicians, NPs, and PAs. They involve panels of experts and moderators.
He is an expert on grant writing. He has helped develop dozens of CME programs focused on public health issues like vaccines for pneumonia, HPV, and the flu.
Of his experience in the DMSc program, he said he found the program challenging and incredibly worthwhile, and enjoyed the research part of the courses the most. What he finds most intriguing about the program, faculty and especially his colleagues are how every single one has adapted to the current crises.
He is proud of how colleagues have responded to the COVID-19 crisis. He borrowed a colleague’s expression: “PAs are the stem cells of medicine. They adapt, grow, and go wherever is necessary. They respond, fill the void, and fix things.”
That is why PAs – regardless of their specialty – were so valuable during the COVID-19 outbreak, he said. The family practice PA can adapt and do telemedicine or fill-in in the emergency department. The cardiothoracic PA is comfortable outside the operating room and managing the intensive care unit (ICU) .
He said that PAs are, without a doubt, the most adaptable healthcare providers during unprecedented times.
 “A career in medicine has been one of my dreams, since childhood,” said Zekharia Idro ’21 DMSc, PA-C. He dreamed of becoming a public servant and organizing medical mission trips to his home country of South Sudan.
“A career in medicine has been one of my dreams, since childhood,” said Zekharia Idro ’21 DMSc, PA-C. He dreamed of becoming a public servant and organizing medical mission trips to his home country of South Sudan.
Idro’s journey to a career in medicine began when he was a child in South Sudan.
“As a child, I saw a lot of trauma, a lot of injuries, a lot of death. There, even with no training, if you see someone in front of you who needs help, you naturally help them. So at a very early age, that experience gave me a level of interest in medicine,” he said.
During the second civil war in South Sudan, he was one of around 4,000 individuals removed from the conflict by the United Nations. He came to the U.S. in 2003.
“Some of my fellow students have made good progress in life. I never imagined that one day I would own a house, I would one day own a car, and be active in my community, and it has been quite a journey,“ he reflected.
He currently practices in an urgent care clinic near Palm Springs, California. The area is considered underserved because there are not enough medical providers compared to the population. Idro likes the versatility of urgent care. He sees around 100 patients every day.
“I see a little bit of everything. It is very satisfying — I enjoy practicing here. We function very much like an emergency room. Unless someone is in a life or death situation, they come to our clinic,” he said.
Idro said he functions very independently as a PA in his practice with three other providers, two NPs, and one other PA. He added during rounds, they depend on their own experience and knowledge to treat patients.
As a student in the DMSc program, Idro said, “Global Health has been interesting — most of my writing has had to do with where I come from, in South Sudan.
“Specifically, I have written about women’s health, children’s health, and sanitation. I count myself and my family as very lucky, because my mother, a mother of nine children, did not suffer as many others have suffered.”
“I have found all of the courses in the DMSc to be very relevant and applicable to my situation. We have learned things about Healthcare Management, [and] how our system works. Each course has been impressive and challenging, teaching you how to think critically and independently,” he said.
Idro said that getting his doctorate fits into his personal and professional long-term goals.
“In the future, I would love to run for office; I want to be a public servant. When I see my patients, and how the system is working with them, I see myself there. I want to advocate for them. When I came to the U.S., I became a citizen, but I still see myself as an immigrant. The system appears to not be working well for the underserved population I see,” Idro said.
He said he sees people dealing with trauma every day, living in an area where hearing gunshots is common and weekly homicides are reported.
“I would love to add my voice to help in this area. I have a goal of being a public servant and doing what I can to help the poor in this community,” he said.
Idro said that one of the main problems with access to care for patients with chronic issues such as hypertension and diabetes is that “there are people suffering here, needlessly, and they need an advocate.”
Idro has another goal as well: to find and mobilize a group of 15-20 medical providers to go to South Sudan.
“We could go to a specific town, perform wound care, treat people with malaria and other conditions — perhaps dentists could go also. It would be a voluntary medical mission We could fundraise, save for the trip, and go for two weeks. They will appreciate it,” he said.
Idro said he was inspired by a friend from Tanzania who organized a trip to Haiti after the Tsunami of 2005.
“People in this country, myself included, often take for granted the things we have here, the freedom to do what we want to do. Life is not just about doing things for yourself. It is about helping other people. Life itself is about others. We cannot exist without others,” he said.
 Col. Amy Jackson PA-C is making history. A couple of years ago, she took command of Keller Army Community Hospital at West Point, becoming the first PA to do so in the organization’s history.
Col. Amy Jackson PA-C is making history. A couple of years ago, she took command of Keller Army Community Hospital at West Point, becoming the first PA to do so in the organization’s history.
Jackson set several priorities for her years in command. Her first priority was to serve her organization.
“I have seen a shift in my leadership style since entering into this role. I am redesigning my style in flight, in order to meet the requirements of my position in this executive role,” she said.
The second priority was providing access to care for the West Point community. Jackson saids a silver lining of the COVID-19 pandemic operational environment was the enhanced use of virtual healthcare delivery.
She said nearly 40% of their encounters are now done online.That is goof for patients because it is more convenient for them to manage their health conditions. Patients may follow up with them by getting a call on their phones.
“Plus, our pharmacy technicians have completed over 7,000 deliveries of medication to the parking lot, thus reducing contact with any potentially symptomatic patients. It is critical that access to care is number one for our patient community. Virtual healthcare appointments have made access possible in the COVID-19 environment,” she said.
 Another priority for Jackson was building community.
Another priority for Jackson was building community.
“I recognize that I am just one person. In order to achieve our institutional goals, we have to work as a team. All of us have to all be rowing in the same direction. Working collectively, we can achieve positive transformation as an organization, and we can take it to the next level. I am focused on creating relationships and building a collective effort,” she said.
She initiated team-building events and a strategic planning conference to identify a strategy for the organization. This helped create opportunities for cohesive relationships.
“We intend to analyze and validate our mission and vision, chart a path to achieve long term goals and objectives, and develop action plans for those goals and objectives,” she said.
Jackson says successful planning for the future at this level begins with an emphasis on culture and people.
“Our people are our greatest asset and strength. The next step in planning for the future is to understand the environment and the mission and vision of our higher headquarters, and be prepared to operate and succeed in dynamic and ambiguous scenarios.
“I recognize diversity is a strength across our organization. The U.S. Army is a true melting pot – we are by nature a diverse organization! We honor all people; we give them the dignity and respect that they deserve as valued members of a squad and team. People need to hear this from their leadership. I decided to share my story with my “squad” so they might understand me, where I come from, and how we share commonality and differences alike,” she said.
Her community forums, called Tree Talks, provide a platform for soldiers to voice any issues they may have noticed or experienced.
“I am genuinely interested in making things better. I am taking the opportunity to meet people in order to make genuine connections. I expect that these connections will afford me the opportunity to take care of those who follow me, as I believe this is why leaders are entrusted with the responsibility and authority of command,” she said.
After just a couple of months, Jackson is off to a running start, representing PAs at the executive level of leadership and medicine.
 Rashadah Jordan, PA-C, PSY-CAQ found that she likes to mentor and teach people early on in her career.
Rashadah Jordan, PA-C, PSY-CAQ found that she likes to mentor and teach people early on in her career.
“I am developing an online coaching program for PAs — there are many potential PA students out there who don’t realize the opportunities available to them in this profession,” she said.
Videos on her YouTube channel, “Reese the Psych PA-C,” describe what life is like as a psychology PA.
Her coaching program started the week of Thanksgiving. It helps students who are applying to PA school. She planned to talk about how to write a personal statement, pick your top five schools, and identify people to write recommendation letters.
“I am passionate about advancing our profession and spreading information about what being a PA is all about. I believe there are a lot of young people out there who would be interested in our profession,” she said.
Jordan works in psychiatry, but she was initially set on becoming a pediatric cardiology PA.
“I was very focused on cardiology until we started digging into studying EKGs. I realized early on that this wasn’t for me. I wanted to move into a different area. I didn’t pick psychiatry — psychiatry picked me,” she said.
Jordan discovered psychology during a behavioral health rotation in her clinical year and fell in love with it.
“I found that I was very good in this field and that it came easily to me,” she said.
As a psychology PA, she has seen an uptick in anxiety levels among her patients. She sees between 12 and 25 patients per day, with a patient population age 5 and up.
“I work with children in group homes, some from detention centers, in foster care, and of course some with very traumatic backgrounds. It is difficult but very rewarding work,” she said.
Jordan performs assessments for medication management and makes referrals as needed for counseling or medical issues.
“My director is a PA, and I work with three other PAs. Our supervising physician has his own practice across the city. I became an advocate because PAs need the authority to practice independently, because it’s what we are already doing,” she said.
She believed the DMSc helped her gain the knowledge to be an advocate for independent practice.
“I want to pursue my doctorate because there are so many avenues presented to advance the PA profession,” she said.
“I have enjoyed meeting the leadership at high levels within the PA profession, and I am learning in this role,” she said.
She was interested in pursuing the executive leadership certificate and wasconsidering the public health certificate.
“Having this body of knowledge will help me communicate in leadership circles on advancing the profession, and disseminating information about PAs to the general public,” she said.
Jordan’s website can be found at www.dreamsinspirelife.com and on Instagram at DreamsInspireLife.
 Adrienne Kramer, PA was thankful for the DMSc program format as it allowed her to also serve a one-year assignment in Kuwait with the Area Support Group-Kuwait (ASG-KU) Deputy Command Surgeon.
Adrienne Kramer, PA was thankful for the DMSc program format as it allowed her to also serve a one-year assignment in Kuwait with the Area Support Group-Kuwait (ASG-KU) Deputy Command Surgeon.
“The program has worked perfectly for me. I have been dedicating my extra time to completing doctoral coursework, instead of focusing on missing my family back home. I was thrilled with the fact that the program can be completed in one year,” she said.
The year away from home was a deciding factor in her enrolling in the program, but she has found that the program also rekindled her interest in publishing in journals.
“Publishing is one of the things you know you should do, but other responsibilities often take priority. The faculty has been exceptional and has supported me all along the way. A particular standout has been Dr. Nancy Reid, my advisor,” she said.
In addition to serving as the ASG-KU Deputy Command Surgeon, she managed the U.S. Army Health Clinic-Kuwait at Camp Arifjan. With nearly 14 years of active duty service under her belt, Kramer advised the installation commander on all health-related interests — planning, monitoring, and implementing Force Health Protection measures like an epidemic response.
“It was truly a unique and interesting situation — how the coursework fit in with the current COVID-19 pandemic,” she said.
In that role, she was the Tricare point of contact for Kuwait and the liaison between U.S. forces and host nation partners facilitating key leader engagements and interoperability.
“The DMSc’s Health Administration Track fits right in line with my duties running the clinic, and in my role serving as a liaison between the multiple medical commands, and tracking trends in the current COVID-19 outbreak,” she said.
She was drawn to a career in medicine from an early age, and the Army has always been a part of her life. Her father was in the Army, and her mother also for a brief time. They lived in Fayetteville, North Carolina, and it was a natural progression for her.Kramer attended Methodist College (now University) in her hometown, to help her family after the death of her father.
“I took advantage of the Health Professional Loan Repayment Program offered by the military, but instead of utilizing the inactive years, all of mine have been active,” she said.
Kramer stated that the opportunities offered to her by her service in the Army have been wonderful.
“I have served as program manager of the Army’s Interservice PA Program (IPAP), and now I run a clinic. And my husband has been incredibly supportive, and our kids are doing great,” she said.
She also served as the liaison between multiple medical commands in Kuwait and the base commander.
 Dr. Dallas Lipscomb’s passion for providing care and compassion to his patients is what led him to open a new clinic in rural Sierra County, New Mexico.
Dr. Dallas Lipscomb’s passion for providing care and compassion to his patients is what led him to open a new clinic in rural Sierra County, New Mexico.
“I had to get back to my roots. I have always had a heart for providing the best care possible to my patients. I love getting to know them as individuals; I believe this is essential to the art and practice of medicine,” he said.
Lipscomb said that his philosophy of providing compassionate care to his patients was reignited during his time in the DMSc, through interactions with other medical professionals. But, his concern for his community and love of his patients led him to pursue his dream of opening a clinic.
“My DMSc classmates were excited about making a difference, and it made me hunger to enjoy that same possibility. I determined this was not possible in my current setting. I had almost retired due to the stress and the grind,” he said. “I wanted to practice medicine the way I was trained —with compassion.”
He is also a strong believer in independent practice for PAs. As a profession, he thought they need to have the ability to function in that capacity for the profession to survive. He has gotten to know many of his patients over time; he has provided primary care to some of them for decades.
“I have these two patients – a couple, retired Air Force, that have been with me since 1992,” he said. “They’re full-time RVers who wanted to spend retirement seeing the country. They swing in to check in with me for blood work. They tell me: ‘This is a really good thing you are doing.’ And they keep coming back. I like to know my patients. I can look at their faces, and see when something is wrong. You have to build trust. This is what I love.”
 Lipscomb refurbished his new clinic on a budget with lots of love and dedication and with help from the community. A former patient, to who he provided care for years, donated framed and matted Bev Doolittle prints. He will also display a prized Bear Kachina print, a gift from his father upon his completing his PA studies. His father told him that the Bear Kachina is the second most powerful medicine man and to him, that is a PA.
Lipscomb refurbished his new clinic on a budget with lots of love and dedication and with help from the community. A former patient, to who he provided care for years, donated framed and matted Bev Doolittle prints. He will also display a prized Bear Kachina print, a gift from his father upon his completing his PA studies. His father told him that the Bear Kachina is the second most powerful medicine man and to him, that is a PA.
“We are outfitting the clinic on a shoestring budget. Our nearly-new exam room tables were going to be discarded from the local hospital, and I bought them at a great price. We are setting our clinic up with the focus of serving our patients. We’re on a budget but everything is looking amazing,” Lipscomb said.
Lipscomb said he has dipped into his retirement savings to open the clinic and has developed a sustainable business plan. He understands it is difficult to survive as an independent practitioner, but he is committed.
“My biggest focus is practicing medicine. Our concern will be on serving our community of 800 residents in town, with 12,000 in surrounding Sierra County. We are in one of the lowest-income counties in the state of New Mexico, and we have a 20% veteran population,” he said.
 The clinic is situated next to two more suites and, as Compassion Care Clinic grows, it can easily expand into the other suites.
The clinic is situated next to two more suites and, as Compassion Care Clinic grows, it can easily expand into the other suites.
“We’re planning on adding another PA or an NP in six months,” he said. “And, an additional practitioner is slated to come in one year to do clinical counseling.”
The adjacent suite has four exam rooms and a laboratory area.He admits his clinic is a bit of an oddity.
“We are based on compassion. The difference between a good provider and a bad provider is indifference,” he said.
His key to successful and holistic patient care is taking the time to listen and evaluate, as well as relying on your experience and knowledge.
He says his family has been a huge source of support in this effort. His wife will work in the clinic, and his son-in-law plans to join the Compassion Care Clinic in the future.
“I will also mention that my parents were two of my biggest fans. My mother was diagnosed with cancer as I started the DMSc program, during the first classes. Dr. Watkins kept encouraging me to hang in there. She was incredibly supportive. ‘Don’t give up!’ My mother made me promise her that I would finish the doctorate. So part of my motivation was to keep my promise to her,” Lipscomb said.
He said the doctorate refreshed his memory of what the practice of medicine is all about.
“Take care of the patient, and the money works itself out,” he said. “It’s got to be about the compassion. We will maintain our altruistic focus throughout this venture.”
 Victoria Louwagie loved her job as a PA and saw the DMSc as a strategic next step in her career.
Victoria Louwagie loved her job as a PA and saw the DMSc as a strategic next step in her career.
“I am very passionate about clinical practice. Long-term, I could see myself going into more of an administrative role. Having a terminal degree as a PA may bring you to a table that you might not have been invited to otherwise,” she said.
Louwagie is an assistant professor with the Mayo Clinic and trains PAs, nurse practitioners, and medical students.
“I loved connecting with other faculty and those that are passionate about medical education,” she states. “We are trying as an organization to entice PAs to pursue academic ranks. There’s emerging research that indicates that practitioners want to do this; we are trying to identify the barriers and gaps that are keeping PAs from the pursuit of academic rank or being promoted within academic ranks.”
She also started a new business Expanding Healthcare Solutions, a healthcare consulting firm with a nurse practitioner. Together they partner towards optimizing and implementing NPs and PAs into clinical practice.
“I can see this trend growing. What we plan to do is partner with organizations and advance the PA/NP professions within clinical practice to increase healthcare access and provide quality care,” she said.
Louwagie grew up in a household exposed to the medical field — her mother is a retired physician.
“I saw how working in medicine brought my mother fulfillment,” she said. “Right now, I love practicing. But I decided to pursue the DMSc because I realized that I needed a terminal degree to move into some additional leadership roles, not only in my organization. I felt the need to stay competitive within my field.”
Louwagie said she feels the coursework and content have been 100% applicable to daily practice.
“I actually completed the healthcare administration certificate first. I really resonated with the healthcare management course taught by Dr. Laura Witte. Based on my excellent experience, I decided to complete the DMSc degree! I found the program to be both challenging and manageable as a busy practitioner and mother to a toddler. Also, the discussion boards have been fantastic. It has been so refreshing to connect with PAs all over the world, we are everywhere and we’re doing everything!” she said.
Louwagie presented “Understanding Academic Rank Among Physician Assistants Practicing in Academic Medical Centers ” virtually at the American Academy of PA’s 2021 conference.
 John Lynch ’21 DMSc, PA-C was excited to start his new career as a clinical team leader with CareTeam. CareTeam is a growing healthcare organization that partners with employers across the country to provide primary care and occupational medicine services to employees and their families. Lynch manages a team of advanced practice professionals including both PAs and nurse practitioners, across 22 CareTeam health center locations.
John Lynch ’21 DMSc, PA-C was excited to start his new career as a clinical team leader with CareTeam. CareTeam is a growing healthcare organization that partners with employers across the country to provide primary care and occupational medicine services to employees and their families. Lynch manages a team of advanced practice professionals including both PAs and nurse practitioners, across 22 CareTeam health center locations.
“My job responsibilities will allow me to make a difference,” Lynch said. “I’ll have a role in helping to standardize procedures within the clinics. I am looking forward to onboarding new clinical team members and making sure they are comfortable with procedures and flow, along with electronic medical records. I will also provide clinical coverage at health centers during special programs and events.”
Lynch was attracted to CareTeam because of their philosophy: “live well, work well.” CareTeam’s health centers encourage an average of 25-minute appointments, so providers can assess whole health needs.
“I’m happy to say that I see eight to 10 patients during an eight-hour shift, and I’m experiencing renewed joy in my clinical practice,” he said. “I have met wonderful people, with lots of good spirit and a positive direction for the future!”
He credits the health administration classes in the DMSc with providing him with the skills he will utilize in his new role.
“I am thrilled that I will be in a role to advocate for the PA profession by example through leadership,” he said.
“The mentorship I have received from my DMSc peer group, as well as the guidance provided in the executive leadership and healthcare advocacy course taught by Dr. Jeremy Welsh and Dr. David Mittman have inspired me. The tools I have gained through the DMSc have proved invaluable,” he said.
Lynch has always been interested in travel medicine and tropical and infectious disease. His 30-year career with the federal government allowed him to explore many different parts of the world and gain experience in emergency planning and coordination.
As Lynch was considering topics to write about for his evidence-based medicine course, he came across articles discussing yellow fever and the vaccine being in short supply. He found this topic very interesting and decided to do more research into it.
“I became very interested in yellow fever, and the vaccine production and its history,” he said.The reservoir of yellow fever is in apes, in the jungle, and every once in a while it will spill out into the countryside. The fear is that the virus – which is transmitted by the same mosquito that vectors Zika virus – if it gets into a village or a city and an urban outbreak occurs, you have a real disaster.”
As he researched, he found a piece by a medical historian that described a yellow fever outbreak in Norfolk, Virginia in 1855. His research on the Virginia outbreak confirmed that the crisis affected Norfolk more than the black plague affected London in 1665.
“As a Virginian, and a history buff, I was very surprised that I had not heard about this before, so I had to pursue the story. “I was stunned – everyone knows about the black plague of London, but not many have heard of the Norfolk yellow fever outbreak,” he said.
Lynch decided to submit his paper topic to the Virginia Academy of Physician Assistants (VAPA) for consideration for their annual summer conference. The paper was accepted and he presented “Yellow Jack: the Reemergence of Yellow Fever”in 2021.
“During the presentation, we discussed the yellow fever vaccine and vaccine production. The vaccine and mosquito control are literally the only things we have to combat yellow fever – similar to COVID-19, everything else is symptomatic treatment,” he said.
His presentation drew from his real-life experiences in emergency planning throughout his career.
Of his experience in the DMSc, Lynch said he was very happy with what he encountered.
“The instructors have been incredible and very supportive. I have enjoyed the class content and also the discussion boards,” he said.
Lynch also noted that the breadth and depth of the experiences of classmates is impressive.
“I am thrilled with the academic rigor of the program, and I enjoy the intellectual conversations with my colleagues in the program,” he said.
 Taisha McIntyre ’21 DMSc, PA-C practices in psychiatry in Florida, and before that worked in pain management.
Taisha McIntyre ’21 DMSc, PA-C practices in psychiatry in Florida, and before that worked in pain management.
“I realized there are so many cases of unmanaged mental health issues in pain management, which led me to psychiatry,” she said.
McIntyre worked in an outpatient setting; she sees children through geriatric patients. She also practices in an inpatient substance abuse rehab facility a few mornings a week.
McIntyre graduated from Duke University’s PA program in 2005 and received her DMSc from the University of Lynchburg in May 2021.
On Advocacy
Of her practice, she said: “My patients often open up to me about [the] care they have received in the past, and I have unfortunately seen a lot of disparities in healthcare. I try my best to empower my patients to speak up, and I also advocate for them whenever I can. PAs can fill a huge gap in advocating for patients and improving outcomes in underserved populations.
“I am first-generation born in the United States, my parents being from Jamaica. And, as I grew up, my family placed a huge emphasis on higher education. My very wise dad had a great quote that has stayed with me all these years: ‘There is nothing worse than getting up every day to go to a job that you hate.’ And, although I was drawn to medicine, the thought of going through years of medical school did not seem realistic to me. It was a big transition going to undergrad. So when I learned about the PA career path, I knew that was for me. I love the flexibility and the innovative nature of this profession.”
McIntyre believes there’s a lot of work to be done in advocacy.
“I am a huge advocate for PAs; I have seen the difference we make as medical providers. However, there is so much more we can do! PAs, in general, are very innovative and open-minded to hearing patients’ input on their route of care, which leads to better healthcare outcomes,” she said.“Even now, at times PAs tend to be closed in boxes by other medical professionals who may not be accustomed to working with our profession. But time and time again, once they see what we can do, they realize our value and how much we offer to healthcare. This is why the DMSc is important to me — it allows the PA profession to have a voice at the table. We need to be able to practice to the full extent of our training and education.”
What’s next?
McIntyre’s interest in yoga has sparked another idea: “I am considering creating a trauma-focused yoga training. The young patients I see in rehab could benefit from this and it could be a tool in helping stop the cycle of substance use disorder.”
She also has an evident passion for empowering a new generation of PAs.
“I love working with first-generation students and students from underserved backgrounds,” she said. “I am also interested in somehow being a part of introducing our profession overseas in Jamaica. I have seen firsthand the need there, and the huge gaps in healthcare. And if I could collaborate to help start a program there, that would be a dream come true.”
 Robert McKenna has a lot of experience in the healthcare industry. He worked as a medical science liaison and MSL manager for over 30 years before he retired from his last role as director of field medical affairs for Radius Health in September 2020. He now brings all that experience to his DMSc cohort.
Robert McKenna has a lot of experience in the healthcare industry. He worked as a medical science liaison and MSL manager for over 30 years before he retired from his last role as director of field medical affairs for Radius Health in September 2020. He now brings all that experience to his DMSc cohort.
“I am now pursuing a career in academia because I believe in the importance of sharing my experience with the next generation of PAs,” he said.
McKenna served as assistant professor of medicine and director of accreditation at Marshall B. Ketchum University.
“Had the DMSc online option existed earlier in my career, I definitely would have pursued it,” he said, noting the relevance of the DMSc in his MSL career.
Nowadays, many biopharmaceutical companies require that MSLs have a terminal degree.
“I found the individuals who were most successful in those roles were those who had a deep understanding of how to read and interpret the medical literature, how professional medical societies work, and importantly, clinical experience,” he said.
“It’s that clinical experience that allowed the MSL to understand and empathize with the clinical leaders and medical scientists MSLs interact with and understand what the science means in terms of what the patient is likely to experience.
“I developed a deep understanding of evidence-based practice, the biopharmaceutical regulatory environment, and how therapies progress from the manufacturers to the patient through experience and on-the-job training,” he said.
He added that if there had been a doctoral-level program that addressed these issues along with MSL field-craft, his career would have progressed more quickly.McKenna said he was thrilled to find Lynchburg’s DMSc, the first of its kind developed specifically for PAs.
“Those who’ve earned a DMSc early in their career will have more options than I did, even with all my experience. This terminal degree for PAs will open so many doors,” he said.
 Joe Newcomb PA-C, is the director of aviation medicine with the National Oceanic and Atmospheric Administration (NOAA). He was voted chair-elect for the Physician Assistant Professional Advisory Group (PAPAG) with the Public Health Service, a role he assumed in 2022.
Joe Newcomb PA-C, is the director of aviation medicine with the National Oceanic and Atmospheric Administration (NOAA). He was voted chair-elect for the Physician Assistant Professional Advisory Group (PAPAG) with the Public Health Service, a role he assumed in 2022.
The PAPAG provides advice and consultation to the U.S. Surgeon General through the Health Services Professional Advisory Committee (HSPAC) and chief health services officer on issues relating to professional practice and personnel activities of commissioned officers in the physician assistant professional discipline.
The PAPAG promotes cooperation and communication among health professionals. This year, the PAPAG will be researching and clarifying the issue of state licenses versus national certification and what dictates PAs’ scope of practice within the PHS.
Newcomb said this is related to their ability to help people during emergencies. They are looking at the barriers that stop them from helping people.
“We are concerned with making sure that PAs ability to provide medical care is based on education and experience,” he said.
“Our commissioned officers are doing amazing things at a very junior rank, flying from Lakeland, Florida, to Bethel Alaska. The unit places them in charge of figuring out the mission’s logistics, how they are going to refuel the aircraft, how they are going to assign crews and scientists, and their transportation. It’s a lot of responsibility.”
Joe Newcomb PA-C medically supports those who study hurricanes, snow melts, and perform coastal mapping.
“The most interesting part of my job is flying through hurricanes. When you come up through the eyewall, you see the blue skies above, and all around you is a wall of violent storm. NOAA has completely geared the WP3 aircraft to fly through these conditions,” he said.
Newcomb’s current responsibilities include ensuring that 300+ NOAA officers are healthy enough to fly these great distances. He is also in charge of their primary care – and most recently, given the pandemic, also evaluated a lot of their families’ issues. PAs are versatile like that.
NOAA is currently sponsoring him through the DMSc to further his education.
He said that everything he learned in the DMSc program helped him in his current job. For example, he was able to install an electronic health record program for NOAA.
He said that he used the methods he learned in his first semester of the DMSc program to develop a viral surveillance protocol. The protocol is now being used by NOAA pilots and aircrew.
“Unfortunately, there is no real social isolation you can do in an aircraft. The pilot and the navigator cannot wear PPE because of the instant need to put on oxygen if the cabin depressurizes, and also the need to be able to communicate clearly at all times. This is why we developed the surveillance program. We test every single person who comes into the building once a week; flyers are tested every five days,” he said.
Newcomb has an aviation background and has been in military service for 34 years. He completed PA school through the U.S. Army and was commissioned in the U.S. Public Health Service.
“Right after PA school, I was sent to the bush in Alaska for two and a half years. In the remote areas of Alaska, there are no road systems connecting villages, and the providers in the community health centers there all function very independently,” he said.
In the Alaskan bush, PAs and NPs function as the 24-hour urgent and emergency medicine providers, along with being the local family practice providers. He explained a great example is that in one day, he did a prenatal exam at 6 a.m., and did a post-mortem exam at 6 p.m. the same day. It is “cradle to grave” medicine, he said.
As far as his future is concerned, Newcomb envisioned a possible return to Alaska.
“I would like to go back to Alaska, work part-time as a PA, and teach health sciences in a community college setting. Again, having a doctorate will be necessary for that. There are a few other possibilities on the horizon, but a doctoral education, specifically the DMSc, fits perfectly into all of them,” he said.
 Hung Nguyen, PA emigrated to the U.S. after the Vietnam war. PA Nguyen says from an early age, he was always drawn to the field of medicine. As a young man, he met a PA colleague and thought, “I want to do this!” And so began his four-decade, multi-faceted PA vocation. Over the course of his career, PA Nguyen has practiced in a wide range of disciplines – primarily in internal medicine and family practice, and also geriatrics, emergency medicine, and GI. He is now retired from clinical practice but he continued his career by completing his DMSc.
Hung Nguyen, PA emigrated to the U.S. after the Vietnam war. PA Nguyen says from an early age, he was always drawn to the field of medicine. As a young man, he met a PA colleague and thought, “I want to do this!” And so began his four-decade, multi-faceted PA vocation. Over the course of his career, PA Nguyen has practiced in a wide range of disciplines – primarily in internal medicine and family practice, and also geriatrics, emergency medicine, and GI. He is now retired from clinical practice but he continued his career by completing his DMSc.
Q: What drew you to the DMSc?
A: I wanted to earn my doctorate. I had a friend who completed the program a few years prior to my matriculating, and he highly recommended Lynchburg’s program to me. I have been impressed with the structure of Lynchburg’s program, and the curriculum has been challenging and perfectly suited to the profession.
Q: What were your favorite courses?
A: Very timely were the Disaster Medicine course taught by Dr. Gregory Davenport, and Global Health with Dr. Elyse Watkins. This past January, we were studying the coronavirus outbreak in Wuhan, and looking at the models, and we predicted the pandemic — we literally watched it happen in the United States. I would add that I am confident that we will be able to overcome the virus, and social distancing is the way to do it.
I also found the interactions with other PAs in my classes to be very enriching. My classmates have been top notch PAs from all over the country, and also overseas. Collaborating with them has added to my academic career immensely. The DMSc program was rigorous, and the curriculum timely and interesting, and addressed current issues in real time.
The DMSc is my third professional degree in PA medicine. I am so pleased that I was able to reach my goal of obtaining my doctorate at this stage in my career. I am so thankful to the faculty for their guidance and support.
Q: What are you seeing in California with the COVID-19 pandemic?
A: The situation is changing every day with the coronavirus — in my state as well as worldwide. As of today, California has more than 10,018 cases after New York, New Jersey, and Michigan in total cases. All the non-essential businesses in California are closed, and Californians are following the national guideline to stay home until April 30, 2020. As of yesterday, the mayor of LA county recommended all Angelinos to wear masks to go out in public. The state wants to reactivate retired health professionals for emergency needs; and I am waiting to see when I will be called. It is essential that we all follow the rule of social distancing and stay home, even if it is voluntary. Otherwise, the infection and mortality rate will exponentially increase.
 John Njenga ’21 DMSc, MPH, PA, was serving as a medical attaché at the U.S. Embassy in Brazil when he enrolled in the DMSc program.
John Njenga ’21 DMSc, MPH, PA, was serving as a medical attaché at the U.S. Embassy in Brazil when he enrolled in the DMSc program.
“As a foreign service medical provider, we spend approximately 30-45% [of our time] in medical practice and the remaining time in management and medical diplomacy,” he said.
During the COVID-19 pandemic, Njenga has met with local ministries of health in Brazil, ensuring that local hospitals are well-equipped. He is also responsible for ensuring that American diplomats assigned to Brazil can get back to the U.S, should they experience a crisis of health not manageable in Brazil.
“Getting U.S diplomats back to the U.S. due to medical necessity is part of my job — which has been complicated by COVID-19 this year,” he said.
Njenga became a PA because “I love the flexibility of this profession. You can make a linear jump from one type of medical practice to another as a PA.” Njenga joined the Air Force in 2011 and also worked in rural medicine, treating underserved patients, and communities.
“I enjoy the increased access to healthcare that PAs provide,” he said.”We are able to treat a wide variety of medical situations. In the foreign service, PAs practice independently. PAs and NPs are known as medical providers (MP). We are collectively referred to simply as foreign service medical specialists when you add doctors, psychiatrists, and medical laboratory scientists. I saw the DMSc as a natural step in my development professionally.”
So far in his foreign service career, Njenga has served or toured over 30 countries.
“My job is a dream. I was born and raised in Kenya, and never thought I would be able to work as a diplomat for the United States,” he said.
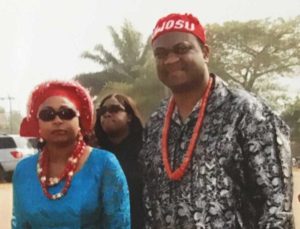 DMSc graduate Jacob Nwosu DMSc ’20, PA-C, has seen an increase in mental health issues during the COVID-19 pandemic.
DMSc graduate Jacob Nwosu DMSc ’20, PA-C, has seen an increase in mental health issues during the COVID-19 pandemic.
“Our practice has gone mostly telehealth, whenever possible. At first this was challenging, given our patient population and the types of services we offer, but we have adapted because that’s what PAs do,” he reflected.
Nwosu practices clinically in psychiatry and substance abuse at a facility near Philadelphia. He says the clinic plans to open back up soon for drug screening and other functions. He notes that besides an upswing in mental health crises, there have also been more domestic violence cases.
“Our clinic has adapted to the situation, we are good at overcoming challenges — but I very much look forward to seeing my patients in person again,” he said.
For many years, Nwosu has spent December and January in Nigeria distributing over 1,000 backpacks filled with supplies to young children in need. He has also coordinated a national Nigerian dance competition for contestants between 14-20 years old. The event has grown in popularity, with some contestants going on to professional careers in dance.
“Humanitarian work is an integral part of my life; I love doing it,” he explained.
This year’s travel plans are questionable, but he says the work can continue without him being present.
“We have been doing this for years, and the events will still happen. I will return another time,” he said.
“My older brother Adam revealed for me my calling to medicine. We were best friends, and one grade apart — we did everything together. And, I watched him start to struggle with substance use, anxiety, and depression when he went away to college.”
 Parins started her journey to becoming a PA at the University of Wisconsin-Madison. After she earned her undergraduate degree, and then her PA master’s degree, she practiced in a variety of specialties — cardiology, orthopedics, and rheumatology.
Parins started her journey to becoming a PA at the University of Wisconsin-Madison. After she earned her undergraduate degree, and then her PA master’s degree, she practiced in a variety of specialties — cardiology, orthopedics, and rheumatology.
“And, then I found my home in internal medicine, with an emphasis on behavioral health,” she said. “I loved it so much because it struck me as an area where you can take care of the whole person.”
She began practicing in an integrated clinic, which took referrals from emergency rooms, patients who did not have regular primary care providers, and individuals struggling with severe mental illness, substance abuse disorders, and chronic pain.
“So often in medicine, we try to separate physical health from mental health, when in reality they overlap substantially and each one affects the other. Our clinic made it a point to integrate behavioral health into all primary care visits,” she said.
In 2016, she joined the University of Wisconsin Madison PA program faculty. There, she was able to share her passion for holistic patient-centered care with her students. This included teaching them about patient-centered communication, trauma-informed care, and health literacy. But, during this time her brother Adam continued to struggle with alcohol addiction, anxiety, and depression. He had back surgery and was prescribed chronic opioid therapy. This progressed into misuse and addiction.
“I watched him struggle with opioid use disorder, anxiety, and depression. I watched him self-medicate. He told me when he took opioids they took away all his pain and all his worries. My family and I tried everything we could think of to help him, but nothing worked. I felt helpless, as a sister, and as a PA, watching the Adam I knew and love disappear,” she said.
Tragically, Parins’ brother Adam lost his battle with substance use disorder.
“The pain from grief took my breath away and brought me to my knees. The days and weeks that followed Adam’s death changed me profoundly. I left my internal medicine practice, and wondered how I could help patients when I felt so broken,” she said.
 A few weeks after Adam passed away, her PA students began their addiction medicine module.
A few weeks after Adam passed away, her PA students began their addiction medicine module.
“Although it was so painful to talk about losing Adam, I knew I wanted to do it. I talked with them about his journey with mental illness and addiction, [and] about what it was like being on the other side of this. People struggling with addiction are still labeled as noncompliant, [and] manipulative due to the manifestations of their brain disease. They are written off and disregarded at times. I want to teach students to meet patients where they are. Ask hard questions, [and] listen —really listen. Then, show up and keep showing up. Our patients with substance use disorders need to be shown respect and given the same care and treatment for any other disease.
“Watching how Adam was treated by the medical community motivated me to speak up. I needed to do something with my pain, otherwise I thought it would eat me alive. Our patients deserve a future without stigma, isolation, or fear. I want our PA students to be equipped with the skills to break down barriers, and treat every person struggling with this chronic disease as a human that deserves respect. For patients with addiction, there is an us-versus-them mentality. This needs to change. This started a big push for my healing,” she said.
Parins began volunteering at a student-run free clinic for underserved, underinsured patients.
“I loved it. It was an opportunity to help people and learn to love medicine again,” she said.
She explained that during her time at the clinic, she started to realize some of the gaps that exist between patient education and health literacy.
“It started to gain momentum wherein eventually I helped our students develop a standardized after-visit summary that optimized health literacy for our patients,” she said.
She now serves as the co-medical director of the Salvation Army MEDiC Clinic.
“The roles reversed— my patients and students helped me heal and find my purpose. I can continue forward. I can keep going,” she said.
 Parins joined Madison Area Care for the Homeless (MACH One) as part of their street medicine team providing direct care to the most vulnerable, unsheltered, and insecurely housed patients in Madison.
Parins joined Madison Area Care for the Homeless (MACH One) as part of their street medicine team providing direct care to the most vulnerable, unsheltered, and insecurely housed patients in Madison.
“Providing face-to-face nonjudgmental care during the pandemic is a gift. Every time I hand out naloxone, I think about how the same medicine could have saved Adam’s life,” she said.
Parins was chosen to be a curriculum content expert at the University of Wisconsin-Madison to develop curriculums for a U.S. Health Resources & Services Administration grant.
“I decided to move forward with my education and training and pursue the doctoral degree to gain more skills as a PA educator, as well as study healthcare advocacy and executive leadership. The focus of my research will be on other ways we can train students to help patients struggling with substance use disorders,” she said.
Her doctoral project focused on how motivational interviewing can help people with substance use disorders, even if the counseling is given by students. “It is really cool to see — seeing that they are as effective as some of the other clinicians in this skill. This really opens avenues and creates a synergistic relationship, where both health professionals [and] students can be really important change agents in their patients’ lives,” she said.
Parins has begun working on the addiction medicine hospital consult team at the University of Wisconsin Hospital, as their first addiction medicine PA.
“This is my calling. It is an honor to help patients when they are at a crossroads.Many know they want to change and want help, [but] others are still ambivalent. Having the tools to help at that crucial moment is profound.
”When you are honest with your patients, they know. When you approach someone with unconditional positive regard and respect, they feel it. It makes a difference. That is a gift I received from Adam — that everyone deserves unconditional love,” she said.
 Dipu Patel ’21 DMSc, PA-C has a unique job as a PA. She works for a healthcare tech start-up as the director of clinical pathways. This means she helps write surgical pathways and educates patients about what to expect before and after surgery.
Dipu Patel ’21 DMSc, PA-C has a unique job as a PA. She works for a healthcare tech start-up as the director of clinical pathways. This means she helps write surgical pathways and educates patients about what to expect before and after surgery.
“As PAs, we are natural educators — we are taught that from the beginning. It’s nice to see a progression, from the face-to-face interactions that we are accustomed to having as frontline providers, to now, in the digital health space, which is where I think healthcare will continue to expand,” she said.
Patel stated that programs like the DMSc allow PAs to continue to add value to the healthcare frontlines, and also in the C-suite and the boardroom.
“More and more of these types of roles are going to become available for PAs to expand their horizons,” she said. “I have been fortunate to have had this role for a year while I was going through the DMSc program. It was extremely fortuitous to be able to hone my skills through the DMSc program while I was actually doing the work — there was definite interconnectivity between the two roles. I was bringing something from my professional job to the program, and vice versa. It was great to bridge both of those worlds.”
Patel said that the use of technology is important for PAs in all areas, including education and hospitals. Patel’s doctoral project titled “Digital Health: Ethical and Policy Challenges” addressed some of these challenges. She also mentioned that her mentor, Lynchburg professor Dr. Mark Archambault, helped her apply her coursework to her unique work setting.
“I can’t say enough good things about Dr. Archambault. He demonstrated such a great willingness to allow me to be outside the box and stay creative in our thinking, especially since I am in a very non-traditional PA role,” she said.
 Patel believed that the DMSc is moving the profession forward. She said PAs are natural leaders and this is the mindset that they need to cultivate in the next generation.
Patel believed that the DMSc is moving the profession forward. She said PAs are natural leaders and this is the mindset that they need to cultivate in the next generation.
“We need to embed this knowledge from the very beginning into our students. Because it is not a lack of ability or creativity or value that is the limiting issue — it’s a matter of having the chance to showcase the abilities we have to offer as PAs,” she said.“I am excited to see what doors this degree will open for me. We should be on equal footing with our other healthcare professional peers and for me, this degree is a step in that direction. We have started down that road, but we are not fully there yet. For anyone that wants to pursue it, I would say go for it!”
When asked what keeps her motivated, she responded, “my kids keep me motivated.”
“Being a single mom, I want to always be the best role model for them and go the extra mile. I want to show my kids that no matter how old you are, you are never too old to learn, you are never too old to love, and you are never too old to lend a hand. And that’s really how I see the PA profession,” she said.
Patel was the 2021 award recipient of the Graduate Doctor of Medical Science Advocacy and Leadership Award. This award honors a DMSc student who is a leader in the PA profession and demonstrates exemplary service. The student must also maintain a high level of academic achievement.

Gabrielle Poole ’21 DMSc, PA-C, stays busy these days, navigating an online learning environment and directing her team from home. In her role as founding program director for the Charleston Southern University’s PA program, she and her team have converted didactic learning for the program’s third cohort of students to an all-online learning environment.
They have also arranged a virtual elective for second-year students who began clinicals in January but were pulled out of rotations due to the COVID-19 pandemic in mid-March. In her spare time, she is also finishing up coursework for her Doctor of Medical Science with a concentration in PA education.
“I never dreamed I would be in the job I currently have. I love my work; I feel fulfilled every day,” she said.
Poole has an obvious passion for education. She always knew she wanted to work in medicine, and the flexibility of the PA world is what drew her into the profession.
“Getting to experience working within many different areas of medicine ultimately drove my decision-making process,” she said.
Of her current position as program director, she said: “this is where my gifts lie — I love planning, organizing, and leading. It’s been the perfect way to use my degree and also train up the next generation of PAs.”
During this unprecedented crisis with COVID-19, she said reaching out to colleagues to share information and support has been crucial. One DMSc classmate is Jenna Rolfs, PA-C, program director for the University of Lynchburg’s School of PA Medicine.
“We have been working very closely together. It has been so valuable to have colleagues in the DMSc program — we have been collaborating on strategies, sharing ideas, and supporting each other during this challenging time,” Poole reflected.
Poole also says that Dr. Mark Archambault, DHSc, PA-C, has been instrumental in her success with the program. She said: “He has provided great insight and feedback to me with regard to developing our PA program and keeping with the guidelines of accreditation. His expertise has been invaluable to me.”
Poole said Archambault encouraged her to pursue the DMSc because it would be a natural next step in her career progression and would complement her day-to-day job extremely well.
“I really wish I had begun the program a year ago — the structure and content of the courses have been incredibly relevant and applicable in preparing us for our second accreditation visit.”
Poole added, “the networking with other PA educators has also been so helpful. Seeing what others are doing and sharing ideas and experiences has been key.”
Of the DMSc program at Lynchburg, she sees the program as relevant for all PA educators.
“As far as increasing understanding of education and teaching, and assessing and evaluating students — you get that in this program. Also, the doctorate degree is often needed for advancement within PA education,” she said.
When asked about her goals for the future, Poole commented, “my biggest goal is to earn accreditation continuation for our program. I am 100% committed to training the next PAs entering the field. I love my job.”
“I have always liked trying and learning new things; I am a lifelong learner. The process of growing and creating new programs and resources — this is what I do,” he said.
Rathke heard about the PA profession during his first time in the Navy during the Gulf War and was drawn to the flexibility of the profession and the ability to move around and focus on a variety of specialties. He said of the PA profession, “I couldn’t think of a better combination of helping other people, serving my country, and having my job be physically making a difference in patients’ lives in a hands-on capacity.”
Rathke’s first job out of PA school was at Yale, after applying for over 200 National Health Service Corps (NHSC) positions, as a site director for a new community health center in rural Fredonia, Arizona.
“We also had a very small nursing home to take care of with around twelve patients,” he said. “As the director, and because it was such a small town, I got to do all of the hiring and PR processes for the community health center. I wrote a monthly news article for the paper; I did PR events like health fairs to get the word out.”
Rathke ended up becoming the president of the Chamber of Commerce and a member of the Fredonia Fire Department during his two years there.
“I was the only medical provider in this amazing and precious rural community, near the north rim of the Grand Canyon,” he reflected.
Rathke’s next move was to practice in cardiology at a naval hospital in Florida, while also starting an information technology education business with colleagues.
“While I was in Pensacola, I met an aerospace physiologist who was active-duty Navy, and this career field sounded extremely interesting,” he said.
With his new mentor’s encouragement, Rathke decided to pursue the Navy career, as flying airplanes was a childhood dream. After being accepted into the aerospace physiology program, he completed three more years of training, which included learning to fly Navy helicopters and airplanes.
“At right about the four-year mark, I really started to miss medicine and taking care of people. I realized that if I continued down this career path, I would be leaving medicine behind me forever. I was not ready to do that,” he said.
Instead, Rathke decided to transition into the U.S. Public Health Service as an active-duty officer and work as a PA again. Since then, he has held three positions within the organization and now serves as director of the Office of Health Services for the National Oceanic and Atmospheric Administration (NOAA).
In this role, Rathke is involved in executive administrative oversight, medical directing, policy writing, and quality assurance aspects for all five NOAA medical programs: aviation medicine, marine medicine, behavioral health, diving medicine, and NOAA Corps medical affairs. Besides this job, for the past 20 months, he has served as medical director for the agency’s COVID-19 response.
“This job has been a privilege. I am grateful to be in the position of writing medical policy — the ripple effect of our policies affects 12,000 people at an agency level in a meaningful and practical way. The policies have the ability to truly move the needle with regard to advocating for the personal health and safety of our personnel within the jobs that they do,” Rathke said.
Rathke also spearheaded a brand new behavioral health program two years ago that has been a huge success. Rathke has testified to Congress twice due to the success of the program, and expansion is planned.
“Our behavioral health program is growing because it is meeting a very real workforce need in a uniquely practical way,” he said.
Rathke says that Lynchburg’s DMSc coursework has been relatable to his daily work.
“On multiple occasions, as I have gone through the DMSc program, I have utilized the information from my classes on the job during the same week that I learned it,” he said.
He noted that the way the coursework is structured requires students to look at the practice of medicine from many viewpoints.
“Lynchburg’s program has been incredibly flexible. I really appreciate the professionalism and mentorship of all the faculty. Dr. Colletti has been a great advisor and has been eager to help with changes in my demanding schedule. I just wish I had done this degree earlier in my career,” he said.
 In 2021, Nancy Reid had a lot to celebrate. She finished her Doctor of Medical Science; her husband Jason graduated with his MBA from Lynchburg later the same day, and daughter Emily finished high school.
In 2021, Nancy Reid had a lot to celebrate. She finished her Doctor of Medical Science; her husband Jason graduated with his MBA from Lynchburg later the same day, and daughter Emily finished high school.
“It has made for an interesting year competing for computers, office space, and bandwidth. I know this has been a common issue for so many during the past year. We had four online learners in the house this year!” she said.
Reid was not only a valued DMSc faculty advisor, associate professor, and mentor, she’s an alumna. Despite having already earned her Doctor of Health Sciences, Reid enrolled in the Lynchburg DMSc.
“I wanted to see what was going on in the other classes – the ones I don’t teach,” she said. “I knew there was a lot of valuable information being shared among cohort members. I especially learned a lot in Healthcare Law — it was tough! I knew there were a lot of interesting discussions going on, and I wanted in on that!”
 Reid found that studying the federal laws that apply to emergency medicine was especially relevant during the COVID-19 situation.
Reid found that studying the federal laws that apply to emergency medicine was especially relevant during the COVID-19 situation.
“It was fascinating to learn about the laws that govern specific areas of practice, particularly when you can transfer a patient. For example, if the [emergency room] is at 100% capacity, what do you do? If the patient is present, you cannot divert them,” she said.
Reid enjoyed the collaboration and relationships formed between members of her cohort.
“We had so many interesting discussion board posts — I think many of my classmates did not know I was faculty — we were all DMSc colleagues!” she said.
Meeting the Moment

“Ten or so weeks back, I was starting my final term of the DMSc and studying Global Health and Disaster Medicine. As I was hearing little bits of news of a novel virus in China, I was simultaneously learning about how we are supposed to plan for such things, and how devastating not planning would be.There was a moment, early in the term, where I began to realize with certainty that the novel virus was going to wind up in the U.S. and that we were wholly unprepared. I began telling my wife, my boss, my medical assistants and front desk, but no one seemed slightly phased by it. I ordered more masks for the office, but a modest amount so I wouldn’t look completely insane, and I began to stock my house with items we would need to survive a siege.
It wasn’t lost on me that what I was studying was perfectly in tune with what I was thinking, and I surely wondered many times if I was allowing my imagination to get the better of me. Nonetheless, as the weeks went on, and the news from China grew more grim, I became more convinced and more diligent with my own preparedness and had to put my faith in our government.
The DMSc has taken my knowledge and education to a whole new level of understanding. And, 100%, I would not have been as prepared for this current situation without the Global Health and Disaster Medicine course taught by Dr. Watkins. I saw what was happening in Wuhan, and we studied the models, and knew what was going to happen here. As a country in general, we were not prepared for this.
After the first cases of what we now know as Covid-19 began to pop up in Washington, it became clear to me that there was no escape, but I still had assumed we had more time. Within a day or two, the news broke that a 50-year-old man was in critical condition in a NY hospital, and that this was not connected to any travel. Here we were looking at a home-grown case of the novel coronavirus. Within an hour or two, my phone began to ring relentlessly. Not only was this case in New York, but it was a half-mile from my home, and a mile from my PA practice.
 The hospital where the patient had been for four days was the same hospital where I sent my patients; many of my patients also work there. Within hours, I learned that more than 100 people were quarantined due to having had contact with this patient, including teachers at my children’s school.
The hospital where the patient had been for four days was the same hospital where I sent my patients; many of my patients also work there. Within hours, I learned that more than 100 people were quarantined due to having had contact with this patient, including teachers at my children’s school.
Since then, my life has not been the same. My kids have been out of school and are stir crazy. My friends and neighbors that I had previously warned about this now assume I know a thing or two and call me all day with questions and anxieties. My 3000+ patients are also very anxious and have been in contact non-stop. Work and this virus have completely consumed my life for the last two weeks, to the extent that I have feared I would not be able to complete the DMSc. Faculty have been so supportive and understanding during this time.
We have been working 10 to 12 hours each day, including fielding calls, and even some office hours late at night and on the weekends. The extra 100 masks I had purchased are gone. We finally reached the point this week where it seemed unsafe to continue to see patients in the office due to lack of protective equipment. We have switched to 100% telemedicine, and currently I feel like we are in a holding pattern.
It’s hard to realize that what is currently happening here in New York, how things have come to a standstill, is not necessarily the norm nationwide. If I had to guess what the future holds, I think the CDC’s estimates are likely accurate. I find the data from Italy and France concerning, but I also recognize that in the US we have something that those countries do not have. We have 140,000 PAs trained broadly in all fields of medicine with the lateral mobility to shift to work in areas of need. If there is a need for thousands of more critical care providers, PAs working in the ED can help fill some of those gaps. The now short-staffed EDs can pull PAs from primary care or family practice to provide urgent and emergent care. The PAs working in dermatology and other non-essential fields can help fill in at the family practice level, refilling medications and providing simple ambulatory care. As a profession, we are perfectly suited to be the difference makers.”
 Jessica Saint-Paul ’20 DMSc, PA, MPH, MCHES is a changemaker. Saint-Paul is a licensed PA, public health practitioner, educator, and philanthropist. She has learned a lot from her 20-year career as a PA. She wants to make it easier for people to get the care they need, so she is serving on the California school-based Health Alliance.
Jessica Saint-Paul ’20 DMSc, PA, MPH, MCHES is a changemaker. Saint-Paul is a licensed PA, public health practitioner, educator, and philanthropist. She has learned a lot from her 20-year career as a PA. She wants to make it easier for people to get the care they need, so she is serving on the California school-based Health Alliance.
“I believe this opportunity is directly related to my doctoral degree. Having my DMSc degree expands my ability to serve in both a leadership and a clinical capacity. This is so much more than just getting an additional degree. I have the ability to directly affect change in health care through population-based medicine,” she said.
Saint-Paul is passionate about her work in adolescent health and medicine, specifically in the area of school-based health care.
“These are their formative years. So many things happen in adolescence. This is when they have the freedom to learn about their own health and develop healthier habits that are taken into adulthood. And now, many of my patients have grown. They are in college, they are parents, and they have used some of the information they received in our exam room that have shaped their lives. It’s amazing to see — I love it!” she said.
 In 2019, Saint-Paul was awarded the Pediatric Physician Assistant of the Year Award from the Society for Physician Assistants in Pediatrics for her dedication and commitment to pediatric patients and the PA profession. She says she was initially enticed by the career flexibility of the PA profession.
In 2019, Saint-Paul was awarded the Pediatric Physician Assistant of the Year Award from the Society for Physician Assistants in Pediatrics for her dedication and commitment to pediatric patients and the PA profession. She says she was initially enticed by the career flexibility of the PA profession.
“As an undergraduate student, I met a PA at Howard University Hospital. Then I looked at the curriculum — I couldn’t believe I could study and eventually practice as a PA in all of these different areas of medicine,” she said. “Our program was extremely rigorous. PAs have always been trained on the medical model, as physicians are. I knew I would see the day where PAs would be respected as partners and clinicians in all areas of medicine. More states like California have pivoted to Optimal Team Practice. It may have taken a pandemic, but PAs have always been able to adapt quickly to opportunities to serve and alleviate medical/health professional shortages.”
 Saint-Paul states she is proud to be a PA because ultimately, PAs are improving access to health care, both locally and globally.
Saint-Paul states she is proud to be a PA because ultimately, PAs are improving access to health care, both locally and globally.
“We are adaptable, we are flexible. Wherever you go to seek health care, you will always find a PA. We are in every area of medicine. We perform histories and physical examinations — provide health education and diagnose and treat patients with acute and chronic medical conditions. We are PArtners in medicine,” she said.
Saint-Paul leverages her experience as a health care worker and her skills in nonprofit management to help students who are interested in working in the health care field. Additionally, she enjoys teaching dual enrollment courses for middle school and high school students who want to learn about health and science-related careers.
“These are our future health care teams,” she said.
Her passion for working in adolescent health led her to found a nonprofit organization in 2005.
“We provide case management and housing for foster care youth. I work with an amazing team providing health assessments and developing policies to assist foster care youth to transition from the dependence of the foster care system to self-sufficiency. And since we have more time with our youth now, they are able to stay in foster care until the age of 21. We provide life skills and help with education and employment, as well as make sure they are getting their physical exams and vaccinations,” she said.
“I am a first-generation Haitian-American. I am familiar with resilience and grit. My parents managed group homes while I was in high school and college. My mother served as a registered public health nurse and my father served as a radiologic technologist. I saw how they were making an impact and this deeply affected me and my decision to become a PA,” she said.
 Jasmina Salcinovic-Spahic ’20 DMSc, who works as a physician’s assistant at a Veterans Affairs hospital in Iowa, bonds with her patients through shared experiences of war. Salcinovic-Spahic grew up in Bosnia, which was embroiled in conflict for four years until she and her family emigrated to the United States as refugees of war in 1997. They started life over in Clarkston, Georgia when she was 15 years old and barely spoke any English.
Jasmina Salcinovic-Spahic ’20 DMSc, who works as a physician’s assistant at a Veterans Affairs hospital in Iowa, bonds with her patients through shared experiences of war. Salcinovic-Spahic grew up in Bosnia, which was embroiled in conflict for four years until she and her family emigrated to the United States as refugees of war in 1997. They started life over in Clarkston, Georgia when she was 15 years old and barely spoke any English.
Of her childhood experience, she said “from an early age, I felt driven to help people through medicine. There was a definite shortage of medical professionals in Bosnia during the war.”
On her decision to take a career path as a PA, Salcinovic-Spahic said that as a young person in Georgia, she worked as a pharmacy tech. A physician introduced her to the PA program at Emory University.
“I was intrigued. I checked it out, applied, and became the only student from Bosnia enrolled in Emory’s program at that time,” she said.
Salcinovic-Spahic moved to Iowa 11 years ago, her husband’s home state. For several years, she has worked at VA Central Iowa Health Care System, with many veterans and said she is always willing to share her personal experiences with them. Salcinovic-Spahic and her patients form natural bonds.
“They are the best patients. They are wonderful, but try to downplay their problems. I love listening to them and getting to know them as people. They inspire and motivate me to work even harder,” she said.
 Salcinovic-Spahic completed her DMSc at the University of Lynchburg in April 2020. She said that the DMSc program was excellent for her. It helped her learn more about medical hematology-oncology, health care policy, and system processes. She also said that the program helped her rediscover her love of writing.
Salcinovic-Spahic completed her DMSc at the University of Lynchburg in April 2020. She said that the DMSc program was excellent for her. It helped her learn more about medical hematology-oncology, health care policy, and system processes. She also said that the program helped her rediscover her love of writing.
She is now driven to publish in journals and loves the community formed with her faculty and fellow DMSc students. Just prior to beginning Lynchburg’s DMSc program, Salcinovic-Spahic completed her Master of Health Care Administration in December 2018 at Des Moines University, all while working full-time and being a mom to two small children.
“I actually cannot believe that I did it all. There is just so much time in the day, and time goes by quickly,” she said.
Upon nearing completion of the DMSc, she was promoted at her hospital and also accepted onto a new Veterans Affairs Board for PAs, which will provide oversight into administrative practices across VA hospitals. In addition, the American Academy of Physician Assistants awarded her the Distinguished Fellow Award . Only 2% of all AAPA members in the country are honored with “DFAAPA” designations.
“I would recommend the program to all PAs who have a passion for professional development and advocating for the PA profession,” she said.
 Gary F. Spinner ’22 DMSc, PA, MPH, AAHIVS has worked to improve the health of underserved populations his entire career. He began caring for HIV patients in 1983 and has spent decades in community health centers as a provider, administrator, and public health advocate.
Gary F. Spinner ’22 DMSc, PA, MPH, AAHIVS has worked to improve the health of underserved populations his entire career. He began caring for HIV patients in 1983 and has spent decades in community health centers as a provider, administrator, and public health advocate.
He provides primary care and treats approximately 450 patients for HIV as well as Hepatitis C.
“I have had the opportunity to speak nationally on HIV prevention, particularly about a medication we call PREP, which stands for pre-exposure prophylaxis,” he said ”People with HIV are disproportionately people of color, and they suffer from stigma. It is vital that they have access to quality, compassionate care. Today, a person who is 20 years old and diagnosed with HIV can live a normal life expectancy if they go on antiviral medication. We have come a really long way.”
Spinner recently authored a chapter of “Fundamentals of HIV Medicine” in which he focused on the similarities between the HIV and COVID-19 pandemics. People of color are disproportionately affected by both pandemics.
 “It is interesting, and it is really no surprise that the same social determinants of health, the same disparities in health care, the same health inequities that people of color have which makes them more predisposed to becoming infected with HIV are the same factors that impact COVID-19,” Spinner explained.
“It is interesting, and it is really no surprise that the same social determinants of health, the same disparities in health care, the same health inequities that people of color have which makes them more predisposed to becoming infected with HIV are the same factors that impact COVID-19,” Spinner explained.
“During my presentation in October to the U.S. Conference on HIV-AIDS, I offered an African-American proverb. [It said] ‘when white people catch a cold, Black people get pneumonia.’ It’s a fitting proverb because [for] people who are disenfranchised, whether you’re looking at diagnoses of diabetes, hypertension, [or] cancer — people who have been victims of systemic racism — there is a huge disparity in outcomes. The COVID-19 pandemic is no different at all.”
Spinner has been caring for people with HIV and AIDS since the start of the HIV epidemic. He became an HIV specialist by getting credentials from the American Academy of HIV Medicine.
As an advocate for improving health care in the developing world, he has global health experience in Nicaragua, Haiti, and Uganda. Spinner believes that everyone should have access to health care. This is important because it will help to end disparities in health between different races, genders, and ethnicities. He believes it can be achieved only by working hard for social justice.
 Keith Stirewalt ’22 DMSc, MBA, MDiv, PA-C became interested in medicine because he wanted to help other people. He is a lifelong learner, so after getting his PA degree in 1984, he went back to school (while working as a PA) to get his MBA. Later on, he helped start an occupational medicine program that worked with four pre-existing urgent care centers. As he was working in corporate medicine for 60-80 hours per week, he realized that he had lost sight of his original goal.
Keith Stirewalt ’22 DMSc, MBA, MDiv, PA-C became interested in medicine because he wanted to help other people. He is a lifelong learner, so after getting his PA degree in 1984, he went back to school (while working as a PA) to get his MBA. Later on, he helped start an occupational medicine program that worked with four pre-existing urgent care centers. As he was working in corporate medicine for 60-80 hours per week, he realized that he had lost sight of his original goal.
“I remembered a call to the ministry that I had long since put to the side,” he said.
Stirewalt left corporate medicine and returned to Wake Forest Divinity School. There, he completed a three-year MDiv degree and became an ordained Baptist minister. He then completed two years of chaplain residency. However, after spending some time in the pastorate, he began to miss the medical environment.
“I was fortunate to be able to take a journey to Israel during my time as a minister. While on the trip, as I was looking out over the Sea of Galilee. I felt a call back to my healthcare roots, where I would be able to blend my call to medicine with my call to ministry,” he said.
Stirewalt soon encountered an opportunity to return to healthcare. He focused on medical education, ethics, and spiritual care for healthcare workers. Stirewalt serves as a resource, creating a safe space for providers to share difficult experiences.
“With organizational support, we have been able to implement Schwartz rounds, where all of our providers can share experiences and are safe to be vulnerable,” he said. “I have seen a need for this throughout my entire career, and it is rewarding to be able to provide this type of service to my fellow providers, whether nurses, PAs, doctors, and chaplains — we all need a safe space.”
Stirewalt completed his Doctor of Medical Science degree at the age of 61. He said this degree expanded his knowledge of global health issues and access to care issues.
“I can look out the window where I am sitting right now, and see the need right here in my community. My goal is to be able to touch as many lives in this community as possible through education, mentoring, and being a resource for my fellow providers,” he said.
Stirewalt attributes much of his success to having a supportive family. His wife, Margaret Norris, is completing her education to become a minister in the Moravian tradition.
“At this point in our lives, where others might be thinking of slowing down, we’re gearing up! We both look forward to these new adventures,” he said.
 Shortly before finishing her doctoral degree, Jessica Wirth ’21 DMSc, PA-C had an article accepted for publication by the Journal of the American Academy of PAs (JAAPA). These are huge accomplishments in their own right, but, Wirth has also had to overcome a brain injury to earn this success.
Shortly before finishing her doctoral degree, Jessica Wirth ’21 DMSc, PA-C had an article accepted for publication by the Journal of the American Academy of PAs (JAAPA). These are huge accomplishments in their own right, but, Wirth has also had to overcome a brain injury to earn this success.
On her journey of recovery to the completion of her doctorate, she said:, “It has been a long road. I went to speech therapy for two years, and I haven’t had a seizure for four years. So it was all just a little hiccup in the road.”
Wirth began that journey by studying exercise physiology in college, having an interest in body movement and orthopedics.
“I originally wanted to go to medical school, but I learned about the PA profession from my father. I was completely drawn in by the flexibility. You can work in different areas according to your interests, or you can specialize,” she said.
Wirth has practiced in urgent care and occupational medicine. Shortly before applying for Lynchburg’s DMSc program, she found a calling to education.
“Teaching is very rewarding, and I also still enjoy working clinically. I absolutely love being a PA!” she stated.
She was drawn to the DMSc by her desire to write and be published. Wirth suffered a serious head injury in the late fall of 2014, shortly after PA school.
“I lost a lot of memory, and I developed expressive aphasia and epilepsy. I thought my PA career was over before it had even begun, she said.
Wirth said that with speech therapy, she improved over time.
“I wanted to prove to myself that I could overcome this! So I enrolled at Lynchburg, knowing I would have to write, and my goal was to be published. So here we are!” she said.
In 2021, Wirth had an article accepted for publication in JAAPA. Her topic was ARFID — Avoidant Restrictive Food Disorder. She explains,
“ARFID is an interesting eating disorder. Most eating disorders are emotionally based — they are based on the perception of body weight, shape, or size,” she said. “ARFID is not at all based on body image; it is based on what the body perceives of food. ARFID is actually quite difficult to treat, because how do you overcome something that your body naturally perceives?”

